
Bladder Cancer
What is Bladder Cancer?
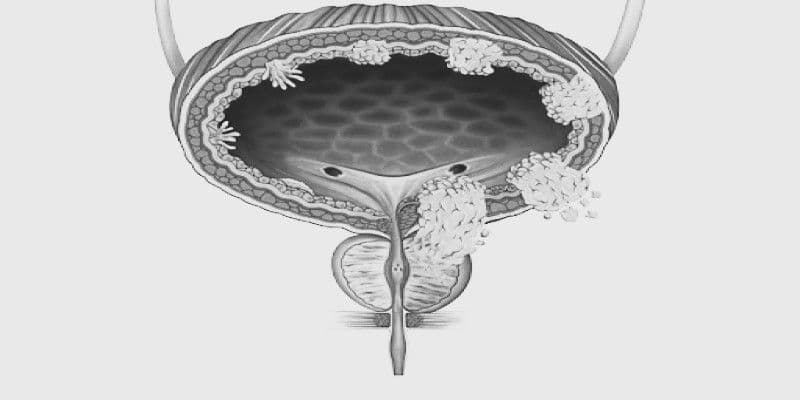
Bladder cancer is defined as when cancerous cells form in the lining of the bladder, the most frequent being urothelial carcinoma, and can vary from non-invasive to invasive types involving deeper layers of the bladder. Bladder cancer tends to present with blood in the urine, increased frequency of urination, and pelvic discomfort and is caused by causes like smoking, chemical exposure, and chronic bladder irritation.
Bladder Cancer Types
Urothelial Carcinoma (Transitional Cell Carcinoma)
•It is the most prevalent type of bladder cancer, starting in the urothelial cells that line the interior of the bladder. It can be low-grade to high-grade and extend to other urinary tract locations, including the ureters and kidneys. It is frequently responsive to surgery and intravesical treatments.
Squamous Cell Carcinoma
•This is a rare type of bladder cancer associated with chronic irritation or inflammation of the bladder, usually induced by prolonged catheterization or repeated infections. It is more virulent and usually diagnosed at a later stage when it is more difficult to treat and results are less optimal than in the case of urothelial carcinoma.
Adenocarcinoma
•Adenocarcinoma arises from bladder glandular mucus-producing cells and accounts for an extremely small fraction of bladder cancer. It is most commonly seen in the setting of congenital anomalies or chronic bladder irritation. Due to its high-grade malignant potential, management is typically radical surgery and follow-up to watch for recurrence.
Small Cell Carcinoma
•This is an extremely aggressive and uncommon bladder cancer that arises in the bladder's neuroendocrine cells. It develops and advances rapidly, frequently outside of the bladder, and necessitates aggressive treatment with chemotherapy and radiation. It is similar in nature to small cell lung cancer and generally carries a worse prognosis.
Bladder Cancer Symptoms
- •
Blood in the urine, usually painless, is the most frequent first sign of bladder cancer.
- •
A painful or burning feeling during urination, which can be caused by a tumor irritating the bladder.
- •
Having to urinate more frequently than normal, particularly at night (nocturia).
- •
An urgent, strong desire to urinate, even when the bladder is not full.
- •
Pain or pressure in the lower back or abdomen that could indicate obstruction or cancer spread.
What’s Notable
Bladder cancer is the ninth most common cancer globally.
Men have a four-fold risk of getting bladder cancer compared to women, particularly those with smoking history.
Bladder cancer has a very high recurrence rate, and hence, a long-term follow-up is required for the survivors.
When to Seek Help
Blood in urine (Hematuria): Even a few drops of blood in the urine—cola-colored, pink, or red—could signal a bladder problem and needs a test right away. Pain on urination (Dysuria): Burning or pain on urination can be a sign of inflammation or a tumor compressing the bladder wall.
Bladder Cancer Causes & Risk Factors
Smoking (Significant Risk Factor)
Carcinogens in tobacco smoke are filtered through the kidneys and deposited in the bladder, causing cumulative damage to the bladder lining.
Exposure to Chemicals at Work
Exposure to dyes, rubber, leather, or industrial chemicals (e.g., aromatic amines) increases the risk of bladder cancer.
Recurrent Bladder Infections or Chronic Inflammation
Recurrent urinary tract infections or long-term catheterization will inflame the lining of the bladder and raise cancer risk.
Age and Gender
Most bladder cancers occur in people older than 55 and are more common in men than in women.
Past Cancer Treatments
Radiation to the pelvis or chemotherapy drugs like cyclophosphamide can increase the risk of getting bladder cancer many years later.
Arsenic in Drinking Water
Consuming large amounts of water containing arsenic can increase the risk of bladder cancer. You or your immediate family members having a history of bladder cancer in your family can reflect inherited risk or exposure to a specific environment.
Bladder Cancer Diagnosis
Initial Symptoms & Check-up
Step 1: Initial Symptoms & Check-up
Blood in the urine, painful urination, or increased frequency leads you to visit your doctor or urologist for assessment.
Your role: Share any changes you’ve noticed openly.
Diagnostic Tests
Step 2: Diagnostic Tests Urine cytology, cystoscopy, and imaging (such as CT urogram or ultrasound) allow visualization and identification of abnormal bladder lining.
Biopsy & Pathology
Step 3: Biopsy & Pathology
A tissue sample during cystoscopy assures the existence, grade, and type of bladder cancer.
Staging & Imaging
Step 4: Staging & Imaging
CT scans or MRI indicates how far the cancer has spreaded—locally or to lymph nodes and organs.
Risk Stratification
Step 5: Risk Stratification
Bladder cancer is staged as non-muscle invasive or muscle-invasive to determine the aggressiveness of treatment.
Personalized Treatment Plan
Step 6: Personalized Treatment Plan
According to your type of cancer, stage, and health, a panel of oncologists and urologists create your personalized care plan.
Step 1: Initial Symptoms & Check-up
Blood in the urine, painful urination, or increased frequency leads you to visit your doctor or urologist for assessment.
Your role: Share any changes you’ve noticed openly.
Step 2
Diagnostic Tests
Step 3
Biopsy & Pathology
Step 4
Staging & Imaging
Step 5
Risk Stratification
Step 6
Personalized Treatment Plan
Bladder Cancer Treatment & Therapy
Chemotherapy
What it does:
Kills rapidly growing bladder cancer cells throughout the body.
Treated for:
Muscle-invasive or metastatic bladder cancer, or before surgery to shrink tumors.
Recovery:
Given in cycles; may cause hair loss, fatigue, and infection risk; needs regular monitoring.
Targeted Therapy
What it does :
Attacks specific cancer-driving molecules to slow tumor growth.
Treated for:
Advanced bladder cancers with mutations like FGFR.
Common medications:
Erdafitinib, Enfortumab vedotin
Recovery:
Personalized to tumor type; fewer side effects than traditional chemo.
Immunotherapy
What it does:
Boosts immune response to detect and attack cancer cells.
Used for:
Advanced or treatment-resistant bladder cancer.
Drugs used:
Atezolizumab, Nivolumab, Pembrolizumab.
Recovery:
May cause fatigue or inflammation-related symptoms; monitored for immune response.
External Beam Radiation Therapy (EBRT)
What it does:
Delivers targeted radiation to destroy cancer cells while sparing healthy tissue.
Treated for:
Patients unable to undergo surgery, or as part of bladder preservation protocols.
Recovery:
Mild bladder irritation, fatigue, or skin changes can occur.
Brachytherapy (Internal Radiation)
What it does:
Places radioactive material directly near the tumor inside the bladder.
Treated for:
Select early-stage bladder cancers or in combination with surgery.
Recovery:
Shorter treatment time; may cause urinary discomfort.
Transurethral Resection of Bladder Tumor (TURBT)
What it does:
Removes early-stage tumors through the urethra without external incisions.
Treated for:
Initial diagnosis and treatment of non-muscle-invasive bladder cancer.
Recovery:
Outpatient; minimal downtime but may need follow-up treatments.
Cystectomy (Partial or Radical)
What it does:
Surgically removes part or all of the bladder to eliminate cancer.
Treated for:
Muscle-invasive or high-grade cancers.
Recovery:
Major surgery; requires urinary reconstruction and post-op rehab.
Urinary Diversion Surgery
What it does:
Creates a new pathway for urine after bladder removal.
Treated for:
Patients undergoing radical cystectomy.
Recovery:
Requires adjustment to a urostomy bag or internal pouch.
Combination Therapy
Goal:
Combines two or more treatments to increase success rate.
What it is:
Chemotherapy with surgery or immunotherapy.
Used for:
Advanced or recurrent bladder cancers.
Recovery:
More intense; requires careful symptom management.
Palliative Care
Goal:
Eases pain, bleeding, urinary issues, and emotional stress.
Used for:
End-stage or unresponsive bladder cancer.
Recovery:
Improves comfort and quality of life.
Recovery
Bladder Preservation
•Bladder-sparing procedures like TURBT with intravesical treatment where needed.
Regular Checkups
•Cystoscopy and urinalysis regularly every few months to identify early recurrence.
Rehabilitation Support
•Pelvic floor exercises and continence management post-surgery or radiation.
Mental Health Counseling
•Psychologists or therapists help to treat body image or anxiety issues.
Peer Support
•Peer groups or cancer navigators to share experience of recovery and emotional support.
Stress Relief Techniques
•Directed breathing, journaling, or meditation to manage anxiety following treatment.
Hydration Schedule
•Maintenance of moderate fluid intake guarantees proper hydration of the urinary tract.
Smoking Cessation
•Smoking cessation decreases recurrence and improves treatment efficacy.
Dietary Adaptations
•Increased consumption of high-fiber, low-fat diet and reduction of bladder irritants like caffeine or hot food.
Bladder Cancer Types
Urothelial Carcinoma (Transitional Cell Carcinoma)
•It is the most prevalent type of bladder cancer, starting in the urothelial cells that line the interior of the bladder. It can be low-grade to high-grade and extend to other urinary tract locations, including the ureters and kidneys. It is frequently responsive to surgery and intravesical treatments.
Squamous Cell Carcinoma
•This is a rare type of bladder cancer associated with chronic irritation or inflammation of the bladder, usually induced by prolonged catheterization or repeated infections. It is more virulent and usually diagnosed at a later stage when it is more difficult to treat and results are less optimal than in the case of urothelial carcinoma.
Adenocarcinoma
•Adenocarcinoma arises from bladder glandular mucus-producing cells and accounts for an extremely small fraction of bladder cancer. It is most commonly seen in the setting of congenital anomalies or chronic bladder irritation. Due to its high-grade malignant potential, management is typically radical surgery and follow-up to watch for recurrence.
Small Cell Carcinoma
•This is an extremely aggressive and uncommon bladder cancer that arises in the bladder's neuroendocrine cells. It develops and advances rapidly, frequently outside of the bladder, and necessitates aggressive treatment with chemotherapy and radiation. It is similar in nature to small cell lung cancer and generally carries a worse prognosis.
Bladder Cancer Symptoms
- •
Blood in the urine, usually painless, is the most frequent first sign of bladder cancer.
- •
A painful or burning feeling during urination, which can be caused by a tumor irritating the bladder.
- •
Having to urinate more frequently than normal, particularly at night (nocturia).
- •
An urgent, strong desire to urinate, even when the bladder is not full.
- •
Pain or pressure in the lower back or abdomen that could indicate obstruction or cancer spread.
What’s Notable
Bladder cancer is the ninth most common cancer globally.
Men have a four-fold risk of getting bladder cancer compared to women, particularly those with smoking history.
Bladder cancer has a very high recurrence rate, and hence, a long-term follow-up is required for the survivors.
When to Seek Help
Blood in urine (Hematuria): Even a few drops of blood in the urine—cola-colored, pink, or red—could signal a bladder problem and needs a test right away. Pain on urination (Dysuria): Burning or pain on urination can be a sign of inflammation or a tumor compressing the bladder wall.
Bladder Cancer Causes & Risk Factors
Smoking (Significant Risk Factor)
Carcinogens in tobacco smoke are filtered through the kidneys and deposited in the bladder, causing cumulative damage to the bladder lining.
Exposure to Chemicals at Work
Exposure to dyes, rubber, leather, or industrial chemicals (e.g., aromatic amines) increases the risk of bladder cancer.
Recurrent Bladder Infections or Chronic Inflammation
Recurrent urinary tract infections or long-term catheterization will inflame the lining of the bladder and raise cancer risk.
Age and Gender
Most bladder cancers occur in people older than 55 and are more common in men than in women.
Past Cancer Treatments
Radiation to the pelvis or chemotherapy drugs like cyclophosphamide can increase the risk of getting bladder cancer many years later.
Arsenic in Drinking Water
Consuming large amounts of water containing arsenic can increase the risk of bladder cancer. You or your immediate family members having a history of bladder cancer in your family can reflect inherited risk or exposure to a specific environment.
Bladder Cancer Diagnosis
Initial Symptoms & Check-up
Step 1: Initial Symptoms & Check-up
Blood in the urine, painful urination, or increased frequency leads you to visit your doctor or urologist for assessment.
Your role: Share any changes you’ve noticed openly.
Diagnostic Tests
Step 2: Diagnostic Tests Urine cytology, cystoscopy, and imaging (such as CT urogram or ultrasound) allow visualization and identification of abnormal bladder lining.
Biopsy & Pathology
Step 3: Biopsy & Pathology
A tissue sample during cystoscopy assures the existence, grade, and type of bladder cancer.
Staging & Imaging
Step 4: Staging & Imaging
CT scans or MRI indicates how far the cancer has spreaded—locally or to lymph nodes and organs.
Risk Stratification
Step 5: Risk Stratification
Bladder cancer is staged as non-muscle invasive or muscle-invasive to determine the aggressiveness of treatment.
Personalized Treatment Plan
Step 6: Personalized Treatment Plan
According to your type of cancer, stage, and health, a panel of oncologists and urologists create your personalized care plan.
Step 1: Initial Symptoms & Check-up
Blood in the urine, painful urination, or increased frequency leads you to visit your doctor or urologist for assessment.
Your role: Share any changes you’ve noticed openly.
Step 2
Diagnostic Tests
Step 3
Biopsy & Pathology
Step 4
Staging & Imaging
Step 5
Risk Stratification
Step 6
Personalized Treatment Plan
Bladder Cancer Treatment & Therapy
Chemotherapy
What it does:
Kills rapidly growing bladder cancer cells throughout the body.
Treated for:
Muscle-invasive or metastatic bladder cancer, or before surgery to shrink tumors.
Recovery:
Given in cycles; may cause hair loss, fatigue, and infection risk; needs regular monitoring.
Targeted Therapy
What it does :
Attacks specific cancer-driving molecules to slow tumor growth.
Treated for:
Advanced bladder cancers with mutations like FGFR.
Common medications:
Erdafitinib, Enfortumab vedotin
Recovery:
Personalized to tumor type; fewer side effects than traditional chemo.
Immunotherapy
What it does:
Boosts immune response to detect and attack cancer cells.
Used for:
Advanced or treatment-resistant bladder cancer.
Drugs used:
Atezolizumab, Nivolumab, Pembrolizumab.
Recovery:
May cause fatigue or inflammation-related symptoms; monitored for immune response.
External Beam Radiation Therapy (EBRT)
What it does:
Delivers targeted radiation to destroy cancer cells while sparing healthy tissue.
Treated for:
Patients unable to undergo surgery, or as part of bladder preservation protocols.
Recovery:
Mild bladder irritation, fatigue, or skin changes can occur.
Brachytherapy (Internal Radiation)
What it does:
Places radioactive material directly near the tumor inside the bladder.
Treated for:
Select early-stage bladder cancers or in combination with surgery.
Recovery:
Shorter treatment time; may cause urinary discomfort.
Transurethral Resection of Bladder Tumor (TURBT)
What it does:
Removes early-stage tumors through the urethra without external incisions.
Treated for:
Initial diagnosis and treatment of non-muscle-invasive bladder cancer.
Recovery:
Outpatient; minimal downtime but may need follow-up treatments.
Cystectomy (Partial or Radical)
What it does:
Surgically removes part or all of the bladder to eliminate cancer.
Treated for:
Muscle-invasive or high-grade cancers.
Recovery:
Major surgery; requires urinary reconstruction and post-op rehab.
Urinary Diversion Surgery
What it does:
Creates a new pathway for urine after bladder removal.
Treated for:
Patients undergoing radical cystectomy.
Recovery:
Requires adjustment to a urostomy bag or internal pouch.
Combination Therapy
Goal:
Combines two or more treatments to increase success rate.
What it is:
Chemotherapy with surgery or immunotherapy.
Used for:
Advanced or recurrent bladder cancers.
Recovery:
More intense; requires careful symptom management.
Palliative Care
Goal:
Eases pain, bleeding, urinary issues, and emotional stress.
Used for:
End-stage or unresponsive bladder cancer.
Recovery:
Improves comfort and quality of life.
Recovery
Bladder Preservation
•Bladder-sparing procedures like TURBT with intravesical treatment where needed.
Regular Checkups
•Cystoscopy and urinalysis regularly every few months to identify early recurrence.
Rehabilitation Support
•Pelvic floor exercises and continence management post-surgery or radiation.
Mental Health Counseling
•Psychologists or therapists help to treat body image or anxiety issues.
Peer Support
•Peer groups or cancer navigators to share experience of recovery and emotional support.
Stress Relief Techniques
•Directed breathing, journaling, or meditation to manage anxiety following treatment.
Hydration Schedule
•Maintenance of moderate fluid intake guarantees proper hydration of the urinary tract.
Smoking Cessation
•Smoking cessation decreases recurrence and improves treatment efficacy.
Dietary Adaptations
•Increased consumption of high-fiber, low-fat diet and reduction of bladder irritants like caffeine or hot food.
Why Choose Everhope For Bladder Cancer?
At Everhope Oncology, we believe that bladder cancer is not merely an illness—it's an individual experience. With our experienced diagnostics, caring attention, and innovative therapies, we're committed to walking with you every step of the way toward healing and hope.
deaths every year in India
new cases globally every year
most common malignancy in India
FAQs on Bladdar Cancer
No question is too small when it comes to your care
No, it can vary from non-invasive (early stage) to muscle-invasive (serious) and both types require different treatment.
Yes, bladder cancer is highly recurrent, which is why lifelong monitoring is necessary.
Not always, but it is a major warning sign that must never be disregarded—it can also signal infections or stones.
Yes, although more prevalent in men, women do get bladder cancer and tend to be diagnosed later because of overlapping symptoms.
Not always. Some cancers in the early stages can be cured without having the bladder removed by using intravesical treatments.
Most cases, particularly if detected early, are very treatable and curable with appropriate therapy combinations.
Find a Centre Near You
Gurgaon EBD 65
EBD 65, Sector 65, Golf Course Extension Road, Gurgaon
